Expert Insights: How to Treat Kidney Disease

We are pleased to present the final article in a three-part series sponsored by The BI-Lilly Alliance and written by Amy Hess Fischl, MS, RD, LDN, BC-ADM, CDCES. Content is provided for information only; please consult with your healthcare provider before making changes to your diabetes management.
So, you have been told you have kidney disease….what now? If you have read the two previous articles, you know that it is possible to slow or stop the progression from getting worse. But how do we do that?
It all depends on where your kidney function is – but the goal is to stop it from getting worse.
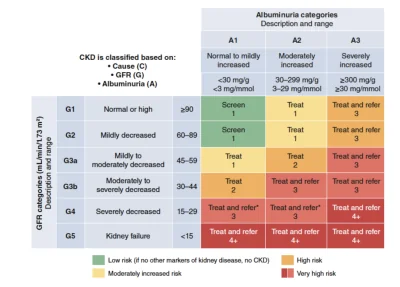
Treatment is based on the five stages of kidney disease – shown in the graphic below (1).
Generally, if kidney disease is categorized as Stage 1 or 2 with UACR <30 mg/g, the main treatment is lifestyle changes and continued screening every 3-6 months.
For all other stages of kidney disease, medicines will most likely be needed.
To reduce the risk of progressing kidney disease, ongoing screening, along with making lifestyle changes, will be your most important assignment.
As kidney function does get worse, there are some signs and symptoms that may occur. Let your healthcare team know of the following changes: (2)
- Swelling in the legs, ankles, feet, face and/or hands
- Change in urination− changes in color and frequency, presence of blood, increased difficulty
- Chills
- Lower back pain
- Unexpected rash or itching of skin
- Lack of energy− fatigue
- Decreased appetite
- Metallic taste in your mouth
- Nausea and vomiting
- Problems breathing− shortness of breath
- Difficulty concentrating, dizziness and problems with your memory
- Waking at night more often
- Decreased urine output
- Weight gain or loss
- Headaches
- Consistently high blood pressure
Delaying Progression
Use the guidelines to keep blood pressure (BP), Urine Albumin to Creatinine Ratio (UACR), estimated Glomerular Filtration Rate (eGFR) and A1C within goals
Key recommendations for screening/monitoring/BP management/A1C targets (1)
| Recommendations | |
| Blood pressure management | IndividualizedFor those with diabetes, high blood pressure and high heart disease risk: <130/80 mmHgFor those with diabetes, high blood pressure, low heart disease risk: <140/90 mmHg |
| Screening/monitoring for kidney disease | At least yearly UACR and eGFR T1D – 5 years after diagnosisT2D – at diagnosisScreen twice a year if UACR is >300 mg/g and/or eGFR 30-60 mL/min/1.73m2 |
| A1C targets | <7% for most people with diabetes6.5-8% range individualized |
Three Ways to Treat for Prevention
Your needs should be reviewed with your healthcare team every 3-6 months. If you are not meeting the BP, kidney screening and A1C goals, adjustments to your medicines may be needed.
1. Healthy Eating
- Make an appointment for nutrition education, specifically known as Medical Nutrition Therapy, with a Registered Dietitian Nutritionist (RDN) to review the nutrition needs that are right for you
- To find an RDN: https://www.eatright.org/find-a-nutrition-expert
- Limit sodium to less than 2000 mg per day
- Protein intake will need to be assessed to make sure you are not eating too much
- An eating pattern high in vegetables, fruits, whole grains, fiber, legumes, plant-based proteins, unsaturated fats, and nuts and lower in processed meats, refined carbohydrates, and sweetened beverage
2. Physical Activity
>/=150 minutes of activity weekly
Try activities like walking, gardening, dancing as well as squats and lunges
3. Medicines
Medicines for blood glucose management, kidney protection and cholesterol should be assessed every 3-6 months.
Newer treatments are available to protect the kidneys – talk to your healthcare team if they are right for you.
You can do things to slow the progression of CKD. The sooner you change your habits, the better!
- Managing blood pressure using the recommendations above as well as individualized goals that are set by your healthcare team
- Maintaining glucose levels within acceptable ranges that have been individualized for you
- Be more active with a goal of at least 150 minutes of activity every week
- Take medicines as prescribed and making sure you are working with your healthcare team every 3-6 months to assess if changes are needed
- Quit smoking
- Follow healthy eating guidelines/see a RDN for Medical Nutrition Therapy
- Reduce stress – there are a lot of way to help us be more calm. Try mindfulness, meditation or guided imagery to name a few.
- Be sure to receive diabetes education, also known as Diabetes Self-Management Education and Support (DSMES) – The 4 Critical Times for DSMES are: (4)
- At Diagnosis
- Annually
- If Complicating Factors Develop
- If Transitions in Life and care Occur
- Use the peer support you have available to you as well through DiabetesSisters, which is a valuable addition to all diabetes education and support
Also, there is a valuable website called “It Takes 2” that covers the basics of kidney disease. You can find it here.
References
DeBoer IH, Khunti K, Sadusky T et al. Diabetes Management in Chronic Kidney Disease: A Consensus Report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Care 2022;45:3075–3090 | https://doi.org/10.2337/dci22-0027.
Alicic R, Nicholas SB. Diabetic Kidney Disease Back in Focus: Management Field Guide for Healthcare Professionals in the 21st Century. Mayo Clin Proc. 2022;97(10):1904-1919.
American Diabetes Association. Chronic Kidney Disease and Risk Management: Standards of Care in Diabetes—2023 Diabetes Care 2023;46(Suppl. 1):S191–S202. https://doi.org/10.2337/dc23-S011.
Davis J, Hess Fischl A, Beck J et al. 2022 National Standards for Diabetes Self-Management Education and Support Diabetes Care 2022;45:484–494 | https://doi.org/10.2337/dc21-2396
Amy Hess Fischl, MS, RD, LDN, BC-ADM, CDCES, is an advanced practice dietitian and diabetes care and education specialist at the University of Chicago within the departments of pediatric and adult endocrinology. She speaks internationally on all diabetes topics, especially meal plan options for type 1 diabetes, insulin pumps,and continuous glucose monitors. She is actively involved in the American Diabetes Association, the Academy of Diabetes Care and Education Specialists, and the Academy of Nutrition and Dietetics, as well as several international groups for diabetes and pre-diabetes. She was named 2018 IL AADE Diabetes Educator of the Year and also received the 2018 Pan Arab Congress on Diabetes Award of Excellence for her contributions to diabetes care and education. Her dream vacation always includes diving with sharks.
Written by